Join our Upcoming Webinar
Previous Webinars
Selected lectures from Kasr Alainy Anesthesia congress
Selected Lectures from BASE 2024
How to use ChatGPT in your clinical practice?
Pain Management
Infections and multi-drug resistance
Fluid Therapy
Mechanical Ventilation
Evidence Based Practice
Anticoagulation
Preoperative Assessment
Sepsis
Dr. Ahmed Mustafa discusses the evolution of spinal cord stimulation (SCS) in neuromodulation, covering its history, mechanisms, and future advancements.




Our Topics in points Summary anytime
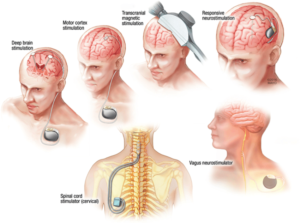
Neuromodulation intervention: The past, present and future of SCS
Dr. Ahmed Mustafa discusses the evolution of spinal cord stimulation (SCS) in neuromodulation, covering its history, mechanisms, and future advancements. Highlights 









Cryoablation: An overview of evidence and clinical use
Cryoablation is a technique using extreme cold for nerve and tissue management, particularly in pain relief, with established clinical applications and evidence. Highlights 











Safety during pain management intervention
Safety in pain management interventions is crucial to prevent harm, minimize adverse reactions, and ensure consistent, reproducible techniques. Highlights 








































